Today marks the 22nd installment in a series of articles by HumanProgress.org titled, Heroes of Progress. This bi-weekly column provides a short introduction to heroes who have made an extraordinary contribution to the well-being of humanity. You can find the 21st part of this series here.
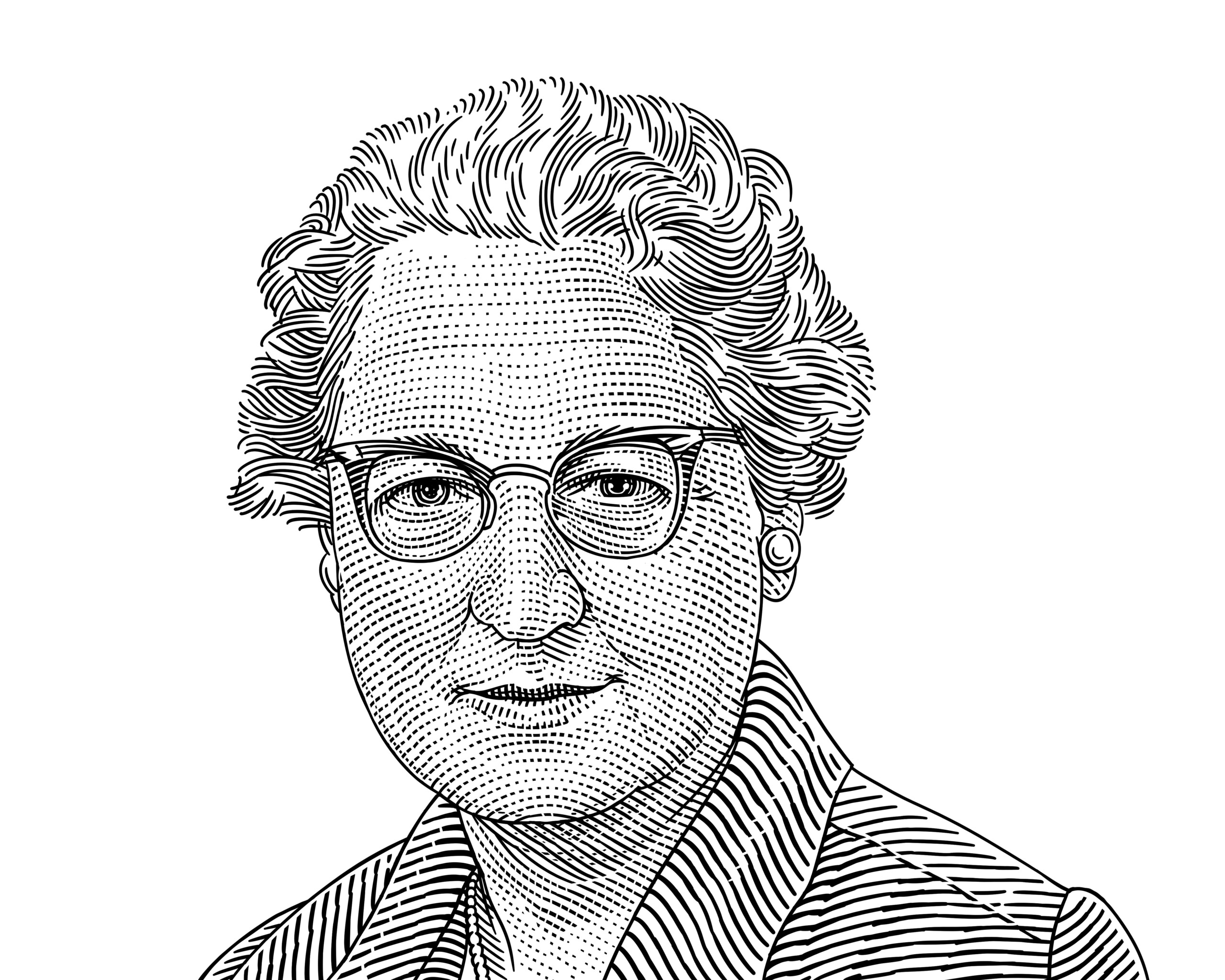
This week, our Hero of Progress is Virginia Apgar, an American anesthesiologist and medical researcher who created a test that is used to quickly assess the health of new-born babies and to determine whether infants need immediate neonatal medical care. The test, which is named the ‘Apgar Score’ continues to be used as a standard practice across the world and it is credited with saving the lives of millions of babies since 1952.
Virginia Apgar was born in Westfield, New Jersey on June 7, 1909. Apgar had two older brothers, one of whom died at a young age due to tuberculosis, while the other lived with a chronic illness. Inspired by both of her brothers’ medical problems, Apgar opted for a career in the medical industry. In 1929, Apgar earnt a degree in zoology with minors in physiology and chemistry from Mount Holyoke College, and in the same year, she began her medical training at Columbia University’s College of Physicians and Surgeons (P&S).
Apgar obtained her MD in 1933 and began a two-year surgical internship at P&S’ Presbyterian Hospital. In spite of her good performance, P&S’ chairman, who was worried about economic prospects of new women surgeons during the Great Depression, advised Apgar to make a career in anesthesiology – a new field of study that was beginning to take shape as a medical, rather than a strictly nursing, speciality.
Apgar accepted the advice and after her internship ended in 1936, she began a year-long anesthetist training course at the Presbyterian Hospital. After completing the course, Apgar performed residencies in anesthesiology at the University of Wisconsin and Bellevue Hospital in Manhattan, NYC. In 1938, she returned to the Presbyterian Hospital and became the director of the newly established division of anesthesia. Apgar was the first woman to hold the position of a director at the Presbyterian Hospital.
In 1949, Apgar also became the first female to hold a full professorship at P&S. Professorship in anesthesiology freed Apgar from many of administrative duties, thus enabling her to devote more of her time to research.
Apgar noticed that infant (i.e., baby between the ages of 0 and 1) mortality in the United States rapidly declined between the 1930s and the 1950’s. However, the death rate for babies in the first 24 hours after birth stayed the same. Perplexed by this discrepancy, Apgar began documenting the differences between healthy new-borns and new-borns requiring medical attention.
In 1952, Apgar created a test called the “Apgar score” that medical professionals could use to asses the health of new-born infants. The Apgar scoring system gives each new-born a score of 0, 1 or 2. Zero denotes the worst possible condition and two denotes the ideal condition across each of the following five categories: activity (muscle tone), pulse, grimace (reflex irritability), appearance (skin color) and respiration. To make her assessment easy to remember, the first letter of each of the five categories spells “APGAR.”
The test is usually performed on new-born babies 1 minute and then 5 minutes after birth. A cumulative score of 3 or below is typically categorized as critically low and a cause for immediate medical action. Apgar’s test soon become common practice across the world. It remains a standard procedure to assess the health of new-born babies today.
In 1959, Apgar graduated with a Master of Public Health degree from Johns Hopkins University and began working for the March of Dimes Foundation – an American nonprofit organization that works to improve the health of mothers and babies – directing its research program with a focus on the treatment and prevention of birth defects.
Whilst working at the March of Dimes, Apgar also became an outspoken advocate for universal vaccinations to prevent the mother-to-child transmission of rubella. Later in life, Apgar became a lecturer and then a clinical professor of pediatrics at Cornell University. She died on August 7, 1974.

Throughout her career, Apgar received numerous honorary doctorates and was awarded the Distinguished Service Award from the American Society of Anesthesiologists (1966) and the Woman of the Year in Science by Ladies Home Journal (1973). In 1995, she was inducted into the U.S. National Women’s Hall of Fame.
The use of the Apgar Score is credited with lowering the infant mortality rate by considerably increasing the likelihood of babies’ survival in the first 24 hours after birth. The invention and use of Apgar’s test has saved millions of lives and continues to save thousands more every day. For that reason, Virginia Apgar is our 22nd Hero of Progress.